Last week, Dr. Truong and I met with a Covidien (now Medtronic) representative who kindly gave us a few boxes of v-loc sutures (3-0 silk, both 90 and 180) and a machine to test tensile strength (pictured below). This week, I will finally begin experimenting with this machine.
 |
(Day 3) This device is what I will be using for tensile testing.
|
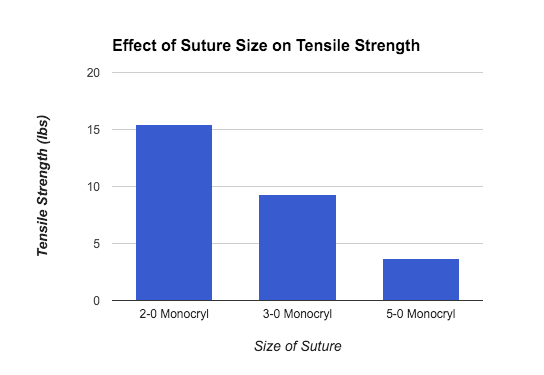
To explain a little more in depth about how this device works, the apparatus functions as the experimenter ties the suture string around the two hooks (using a square knot, for example). The machine is then ‘zeroed’, and we begin to twist the knob on the right, to pull that (right) hook away from the center. As the knob is twisted more and more, the amount of tension in the suture strings is measured (and displayed on the screen). Once the string snaps, the peak tensile strength can be retrieved by pressing the middle button. As I continue with my project, I will be relying heavily on this device to compare the strength of different sutures. After receiving the 2 boxes of V-loc sutures, I began experimenting on the tensile strength device and conducted several trials, using several different types of sutures already available at the office. More details (and some data) to come in the next post!
In terms of observing this week, on Tuesday I was able to watch 3 procedures! Dr. Truong was on call throughout the day and I was able to watch a couple of operations in the morning.
The first operation was to remove a renal mass. Dr. Vegunta and Dr. Truong had to remove a tumor growing around the kidney. The mass had had grown to be larger than the kidney—this may seem surprising, but since the patient was a newborn, the tumor (and kidney) were both very small. Still, this took about 2 hours as the arteries/veins surrounding the kidney had to be found and tied off.
Next, I was able to observe a laparoscopic pyloromyotomy. This procedure is needed for patients with pyloric stenosis. Pyloric stenosis is a condition that usually occurs in newborns and involves the thickening of the pylorus muscle. This leads to a narrowing of the passage between the stomach and the small intestine.
The condition causes vomiting and thus leads to loss of HCl (stomach acid) and dehydration. Because of this, patients must go through ‘fluid resuscitation’ (or replacement) before the operation itself and satisfy certain potassium, sodium, and chloride levels.
Three incisions were made to complete this laparoscopic procedure: one in the belly button, and two slightly higher, on both sides of the midriff area. A laparoscope (camera attached) was inserted through the belly button. With the camera’s video, they were able to locate the stomach, then the connection between the stomach and small intestine. (Find out more about laparoscopic procedures here.) Dr. Truong used a bovie (electrosurgical device) to mark where to cut, then pierced the muscle, using clamp to separate it.
 |
| What a bovie looks like. |
The goal of the procedure is to cut the muscle so that what used to be an ‘O-shaped’ cross-section will now be ‘C-shaped’ (see picture below). This will allow for the passage of formula/breastmilk from the stomach into the rest of the digestive tract. This was the first laparoscopic procedure I’ve seen and definitely the most interesting operation I have observed so far. To read up more about pyloric stenosis, click here.
In case you didn’t notice, that was only two procedures. The second operation I watched involved inserting a drain to remove fluid from an abscess, a process I will explain in my next blog post :^)
Have a great weekend!!
Vanessa